myHIN Blog
Category: Health Disparities Articles

July 05, 2022
Bias in not just in HealthCare: Algorithmic equity in the hiring of underrepresented IT job candidates
published in Online Information Review, Special Issue on Social and Cultural Biases in Information, Algorithms, and Systems by Lynette Yarger, Fay Cobb Payton, Bikalpa Neupane; picked up in IEEE Spectrum Feature
#AlgorithmicBias #AI #Bias #TalentManagement #Tech #DesignJustice
Share

June 13, 2022
Managing Hypervisibility in the HIV Prevention Information Seeking Practices of Black Female College Students
published in Journal of the Association for Information Science and Technology by Lynette Kvasny Yarger and Fay Cobb Payton
#HealthCare #UX #InformationSeeking #BlackWomen #Hypervisibility
Share

December 09, 2015
Decisions, Decisions: Sexual Health Education or Mental Health
Public Health Education is such a broad field of study, with a vast selection of areas to choose from. There’s tobacco, global health, epidemiology, climate change and a host of others. Out of these various topics, I find myself drawn to a few that seem to peak my interest: Sexual/Reproductive Health education, Domestic Violence, and Suicide/Depression. I haven’t decided exactly which area I want to focus on after graduation, but I have tried to educate myself on these topics.
My interest in Sexual Health came about in my Human Sexuality class that I took my first semester in the Health Education department. At first I only took it because I just need another health elective to take and didn’t think anything of it. We discussed so many things in that short amount of time and I was hooked ever since. My professor has been very influential in my decision to teach sexual health education.

On the weekend of November 21st, I had the privilege to volunteer at the 10th Annual Teen Talk Lock-In for the Wake County Health Department. It was an all night, interactive sexual health education workshop for teens. The key areas of focus were attitude & mindset, healthy lifestyles, and access to resources. They had 5 workshops on building positive and healthy relationships, coping and looking forward to positive outcomes, what love is and how to communicate your love to others, understanding your body inside and out, respecting different lifestyles and identities, and also the importance of Sexual Health Education and HIV/STI testing. I was able to go from session to session with the kids and observe the different speakers, my professor being among them. Seeing them interact with this age group, 12 to 17 year olds, further convinced me that I need to do sexual health education. I would like to further help in the fight to make sex a normal thing to talk about in everyday conversation.
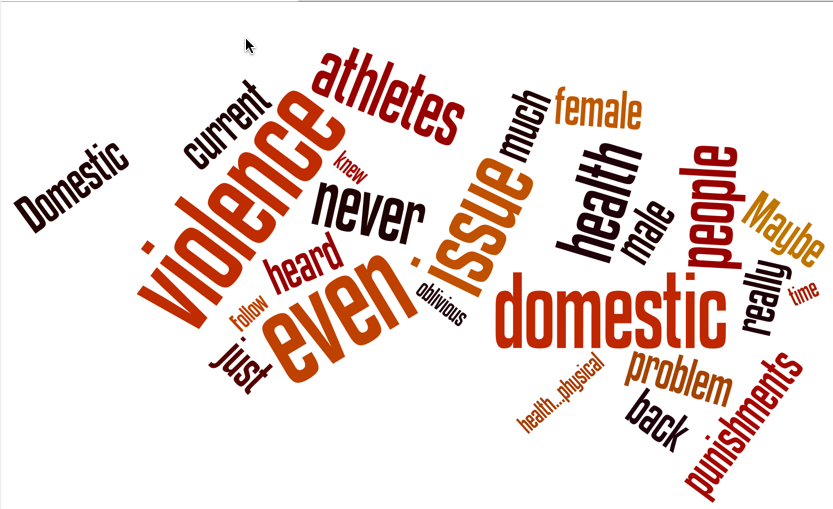
October was Domestic Violence Awareness Month, and I was appointed Chair of the 2nd Annual Women’s Empowerment Program for our Department of Health Education at North Carolina Central University. The purpose of this year’s program was to increase awareness of Intimate Partner Violence (IPV) and its correlation to HIV incidence among college women, through education, empowerment, and condom usage. The goal of the program was to empower young college women to RESPECT themselves in order to PROTECT themselves from HIV. Our keynote speaker and founder of Healing after Domestic Violence (HAD). Her story was so powerful, there wasn’t a dry eye in the house. The program targeted 18 to 24 females on campus. Being in the city of Durham, the young ladies on campus are bound to meet and maybe even start relationships with boys on campus as well as from the surrounding areas. For many of these girls, it is their first time away from home, without direct supervision, and they are likely to take advantage of that. Unfortunately for them, not everyone they deal with will have their best intentions at heart. What can start out as a sweet and loving relationship, can go really south, really fast. The program highlighted signs of domestic violence and where to seek help. There were also booths set up, by myself and my fellow Public Health Associates, showcasing different Social Marketing campaigns focused on Intimate Partner Violence. Resources that are available on campus also had booths set up.

In my research class, we had to choose a health topic to do research on. Normally, I would chose HIV/AIDS, but this time I did suicide and depression, focusing on African American women. I was very surprised that it was hard to find almost any articles on my target population. I’m talking about hours and hours of searching for an article even remotely focusing on depression or suicide in African American women. It was alarming to me, and made me think why no one had decided to do any research on this underserved population, in this regard. As a part of the aforementioned population, I personally know that depression is real in the African American community. There is also a stigma attached to it. I’ve heard people say “Black people don’t get depressed. That’s only crazy white people. Just get over it.” What people don’t realize is that downplaying anyone’s feelings of depression is not helping them at all, and possibly even worsening it, leading them to suicide. If I were to choose this as my final area of focus, I would definitely want to go into research regarding African American women and teenagers.
I wasn’t sure how Public Health Education was going to work out for me when I first transferred to the department, but I soon found my place. I chose to focus on these topics for various reasons. I know people who don’t know how some STIs are transmitted and don’t know how to use condoms properly. I know others who have been in abusive relationships, not even realizing that they were in one, and not want help trying to leave the person. That hurt me, that as their friend, they didn’t want me trying to help them. I, myself, struggle with my own depression, and dealing with it. There is always someone who needs public health education and resources, and as a future health educator, I am working hard so that one day I can help others with their problems.
Follow @myhealthimpact on health and tech stories impacts #youngppl. #publichealth #mentalhealth #sexualhealth
Share

July 15, 2015
Access to Health – A Privilege - and Two Brothers Planning to Collaborate
When I was growing up, eating healthy and physical fitness was something that was talked about fairly often in my household. I played sports throughout my childhood and remained very active. And for the most part, this was the case for everyone in my family. I always had access to a gym, fresh fruits and vegetables. Having the ability to eat healthy is a luxury, and I never really realized how much of a privilege it was until I was exposed to some statistics. “A recent multistate study found that low-income census tracts had half as many supermarkets as wealthy tracts. Another multistate study found that eight percent of African Americans live in a tract with a supermarket, compared to 31 percent of whites” (Bell). I would love to say that a statistic like this really stands out but it doesn’t at all. Minorities, particularly African-Americans, as a community, are extremely disadvantaged when it comes to healthcare as compared to their white counterparts.

When I first began to understand the notion of health disparities, I was intrigued and motivated. Why should citizens of the United States already a decade and a half into the twenty first century not have access to supermarkets close to their places of residence? Over time, I have realized that this is something I would like to change. Closely approaching my senior year of college, I have had the privilege of completing two ethnographic studies that examine pharmacy and supermarket access as well as examining health related racial disparities. Both of these studies examined the neighborhood of East Liberty in Pittsburgh, Pennsylvania which according to 2013 census data is around 74% Black/African-American.
I feel so personally invested in the discussion of healthcare disparities and healthcare equality for all because I identify with the Black/African-American community. After college ,I would like to further my knowledge on these subjects by pursuing my Masters degree in public health. I believe my future education will give me not only the tools and resources to think of potential solutions to my community’s problems but also allow me to work with other like-minded individuals.
One of the like-minded individuals I hope to work with in the future is Marcel Souffrant. Marcel and I went to high school together and have been close friends since around 2011. He is currently planning to attend medical school following graduation from college in the spring of 2016. In a true collaborative effort, I believe we can both help craft potential solutions to these healthcare disparities that currently plague the Black/African-American community. Two Black/African- American men working together to create solutions to these chronic issues is something I am really beginning to like the sound of. Follow the journey along at @myhealthimpact for this, other health-tech topics and voices of young people like me and Marcel.
Citations
Bell, Judith, Gabriella Mora, Erin Hagan, Victor Rubin, and Allison Karpyn. "Access to Healthy Food and Why It Matters." Thefoodtrust.org. Policy Link, 2013. Web. 10 July 2015. <http://thefoodtrust.org/uploads/media_items/grocerygap.original.pdf>
Share
March 01, 2015
MyHealthImpact Topics 2015
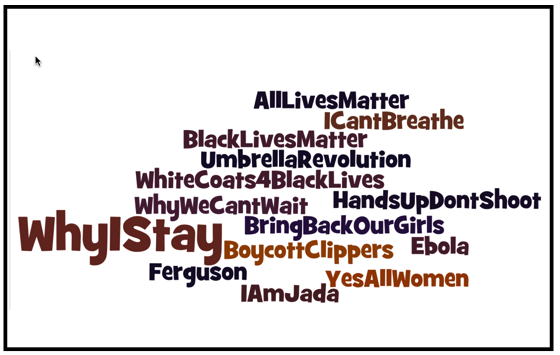
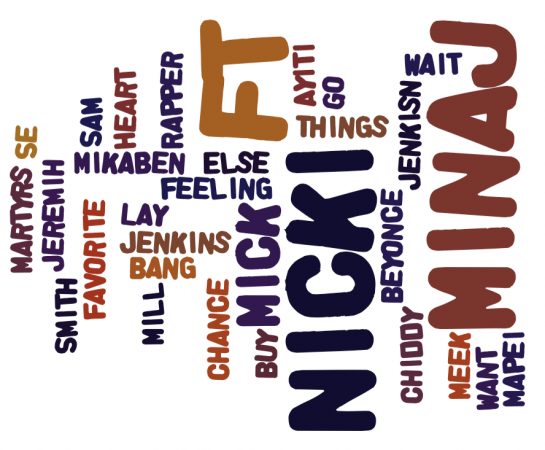
Click on the word clouds below to see a recap of the wonderful blogs by our Research Team so far in 2015.
Stay tuned to @myhealthimpact for more news on the interconnection between health and tech!
Share

April 30, 2014
Empower Me and Health
Recently I started my own blog called ”Empower Me.”. My decision to start a blog came from having a need to just get it all out. Often times, I find it hard to verbalize what I need say but writing these things out seemed to be my way to vent. For the longest, I struggled with a blog name, the audience I wanted to reach, really even if I wanted to go forward with the whole thing, did I have time and would people really read what I have to say? I obviously put those things aside, stepped out on faith and onward I went. As my “about” states, “My goal is to empower and my purpose is to help. I’ve realized that as I pour myself into others, I’m doing nothing but helping myself. Empowering you as I empower myself; uplifting together”. If you can’t tell already, this blog is like my baby. Excuse me, as I get a little passionate. I’m still in the beginning phase of this and I haven’t written many posts but I believe this is the start of something great.
As of yet, I haven’t directly made a post about health and its importance but with my interest and own personal struggles with weight-loss, eating right etc., it isn’t far off. People tend to forget that mental health is a huge component of overall health. I’ve never really thought about it in this way, but I do believe that my blog caters to being mentally healthy; burden-free, honest, successful, stress-free, excited about life and happy. I’m promoting these behaviors because in my own personal opinion, it’s important to be this way. If you haven’t checked out my blog please do so and hopefully it will help you as much as it helps me. Uplifting together.
http://empoweredbykeiara.wordpress.com
Share

October 21, 2013
Health Literacy?
Health Literacy is defined as the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions. It requires a complex group of reading, listening, analytical, and decision-making skills, and the ability to apply these skills to health situations. For example, it includes the ability to understand instructions on prescription drug bottles, appointment slips, medical education brochures, doctor's directions and consent forms, and the ability to negotiate complex health care systems. When patients are faced with complex information and treatment decisions, there are specific tasks that should be carried out to ensure that one is getting the best treatment possible. Those tasks include:
• Evaluating information for credibility and quality
• Analyzing relative risks and benefits
• Calculating dosages
• Interpreting test results
• Locating health information.
In order to accomplish these tasks, individuals may need to be:
• Visually literate
• Computer literate
• Information literate
• Numerically or computationally literate
• Oral language skills are important as well.
In addition to that, it is important for patients to articulate their health concerns and describe their symptoms accurately. They need to ask pertinent questions, and they need to understand spoken medical advice or treatment directions. In an age of shared responsibility between physician and patient for health care, patients need strong decision-making skills.
Next time you visit your local physician, make sure you are practicing and carrying out these tasks. It is important for patients to receive the best care possible, as well as, know how to make accurate decisions when it comes to healthcare.
Follow us on Tumblr tumblr.myhealthimpactnetwork.org
Follow us on Twitter @myhealthimpact
Share

October 21, 2013
Breast Cancer: Study Results, Causes, and Health Literacy
When thinking about breast cancer, many people automatically shift their focus to women. In particular, women within the African American community. Studies have shown that breast cancer is more common in white women than African American women. In all actuality, men are also susceptible to breast cancer. Just like women, men do have breast tissue, which has the possibility of developing breast cancer.
I was pretty surprised when I learned of this news. From my research, the exact cause of breast cancer is not known. Even though there is no exact cause, the risk of getting breast cancer increases with age. Factors such as family history and alcohol usage also increase the possibility of getting breast cancer. For males, the most cases for breast cancer have been detected between ages 60- 70. Overall, a male’s risk of obtaining breast cancer is only 1%. Though this percentage is fairly low, this doesn’t completely eliminate the possibility for men.
In terms of health literacy, everyone needs to be knowledgeable about breast cancer. Having this knowledge base can help improve the quality of life by recognizing the signs early and seeking treatment if necessary. Knowing that breast cancer is 100 times more likely in women than men, this encourages me to consistently check on the women in my life. It is my duty to ensure that they are going to get mammograms and maintaining a healthy lifestyle. Just knowing about breast cancer isn’t enough. Being proactive in your efforts can help save lives.

Follow us on Tumblr tumblr.myhealthimpactnetwork.org
Follow us on Twitter @myhealthimpact
Share

August 28, 2013
Unconscious Bias and Your Health
Almost one year ago, I presented to a group of black female college students on the topic, “You Ain’t Crazy: It’s Your Mental Health”. The sisters wanted to have a frank discussion around dealing with the stress associated with day-to-day issues, such as matriculation at a predominately white institute, culture, family, sexism, racism and how life plays out. Responding to the pressures of it all, one student was asked why did she seek help with her issues, and her response was simple: “to make sure that I don’t go crazy”. One point of frustration highlighted by these students was the interplay between perception and reality. There was the constant practice of second guessing their decisions, particularly scenarios dealing with race and culture. After all, who wants to read more into a situation than is there? You know the questions: “Did he mean to say that? What does he mean? How should I take what was said? How would you perceive that?”
 Reading the situation is a complicated topic, or is it? Dr. David R. Williams, professor of sociology and public health, discusses the topic of unconscious bias in the lives of Black Americans in the September 2013 issue of @essencemag. The two-face depiction captures the article’s title, “No, You’re Not Imagining It”. Williams offers a myriad of scenarios that often causes pause. That is, as a Black person, “Is this really happening to me?”. The element of surprise can grip Black folks though the bias imparted by whites can be unintentional. Yet, the outcome or reality of the scenario can have a profound effect on the recipient. Scholars define unconscious bias as the understanding that people can consciously believe in equality while simultaneously acting on subconscious prejudices they are not aware of.
Reading the situation is a complicated topic, or is it? Dr. David R. Williams, professor of sociology and public health, discusses the topic of unconscious bias in the lives of Black Americans in the September 2013 issue of @essencemag. The two-face depiction captures the article’s title, “No, You’re Not Imagining It”. Williams offers a myriad of scenarios that often causes pause. That is, as a Black person, “Is this really happening to me?”. The element of surprise can grip Black folks though the bias imparted by whites can be unintentional. Yet, the outcome or reality of the scenario can have a profound effect on the recipient. Scholars define unconscious bias as the understanding that people can consciously believe in equality while simultaneously acting on subconscious prejudices they are not aware of.
Williams and other public health scholars have determined that the outcome is not a mere sense of challenge of the parts of Black people. As noted in the Essence piece, someone who  fosters and imparts racial prejudices can do so implicitly; though often automatic, the unconscious bias behavior leads to differential treatment – without effort. Unconscious bias influences the lives of Black people in the form of employment (hence, economic), educational and yes, health and health disparities – albeit heart disease, hypertension, diabetes, obesity, engagement in sexual risk behaviors and depression. While the scenarios offered by Dr. David R. Williams represent every day life as we move about, the resulting questions are commonplace but thought-provoking: “Do you see me? “, and if you do, “how do your see me? In health care, public health scholars ponder the same questions. The relevance here is how you see me starts the dialogue of how your treat me as a person and as a patient.
fosters and imparts racial prejudices can do so implicitly; though often automatic, the unconscious bias behavior leads to differential treatment – without effort. Unconscious bias influences the lives of Black people in the form of employment (hence, economic), educational and yes, health and health disparities – albeit heart disease, hypertension, diabetes, obesity, engagement in sexual risk behaviors and depression. While the scenarios offered by Dr. David R. Williams represent every day life as we move about, the resulting questions are commonplace but thought-provoking: “Do you see me? “, and if you do, “how do your see me? In health care, public health scholars ponder the same questions. The relevance here is how you see me starts the dialogue of how your treat me as a person and as a patient.
As I reflect on recent life circumstances, I ponder my own moments of unconscious bias experiences. There I am in the supermarket as I shop for the next family dinner. The checkout clerk pauses, looks and proceeds to ask me: “Why is your hair so short? Are you a cancer patient, or are you making a statement?” Now, the picture shown here is not I, but the style is one that I own. I am not making a statement nor am I a cancer patient. The politics, bias and perceptions of Black hair, particularly for Black women, is a subject reserved for a read of Dr. Lynette Kvasny’s blog, Black Women’s Love Affair with Hair”. Yet, the very question and judgment (“or making a statement, cancer patient) speaks volumes. My response to the clerk was “what if I am a cancer patient?” His apologetic comments followed as I completed my transaction.
shop for the next family dinner. The checkout clerk pauses, looks and proceeds to ask me: “Why is your hair so short? Are you a cancer patient, or are you making a statement?” Now, the picture shown here is not I, but the style is one that I own. I am not making a statement nor am I a cancer patient. The politics, bias and perceptions of Black hair, particularly for Black women, is a subject reserved for a read of Dr. Lynette Kvasny’s blog, Black Women’s Love Affair with Hair”. Yet, the very question and judgment (“or making a statement, cancer patient) speaks volumes. My response to the clerk was “what if I am a cancer patient?” His apologetic comments followed as I completed my transaction.
Case 2: I had a medical procedure done which was a high stress experience . The waiting for the test results was heave, scary and a prayerful time. During the film read with a physician, I stated aloud” “the mass has a meniscus”. To which the physician replied, “how do you know that? How do you know meniscus? How do you know this? This surprises me”. His surprise momentarily precluded the focus on my medical care. My simple reply to his disbelief was “Chemistry 101 Lab and can we focus on my health”.
Then, there is the unconscious bias imparted in the workplace, the unconscious  organizational impact. This level of bias creates an organizational culture that permeates bias rather intentional or unintentional. This mini-me culture can reinforce bias. This can create personal stress particular in hostile workplace environments. The “I understand; I am sorry”, conjectures do little to offer individual support or reduce health stressors. As one sister indicated in that August 2013 session, “Don’t let them steal your joy”.
organizational impact. This level of bias creates an organizational culture that permeates bias rather intentional or unintentional. This mini-me culture can reinforce bias. This can create personal stress particular in hostile workplace environments. The “I understand; I am sorry”, conjectures do little to offer individual support or reduce health stressors. As one sister indicated in that August 2013 session, “Don’t let them steal your joy”.
As Dr. David Williams offers in the @essencemag article, there are others ways to confront these scenarios. Taking care of your health tops his recommendations. Be resilient, and visualize positive outcomes. Breathe. Pause. For as much I share this advice, am I talking to myself? Yes, constantly. After all, it is my (@myhealthimpact) physical and mental health to protect.
Share

July 30, 2013
Why I Joined the MyHealthImpact Team
It seems like yesterday that I was sitting in Dr. Payton’s Information Systems Management Class alongside my friend, Keiara Morris. I was immediately intrigued when I noticed that Dr. Payton and I shared the same last name “Cobb”. Not many people have Cobb for a last name. After about the second week of class, I went and introduced myself at the conclusion of class. Dr. Payton, too, found it interesting that we shared the name, Cobb. If I can remember correctly, we began to ask where our families were from and made small talk from there.
As time passed, it became second nature for me to go speak to Dr. Payton after class. Keiara and I would go stop by her office hours after class just to chat, and that’s when Dr. Payton introduced me to myHealthImpact. I knew I wanted to become involved when Dr. Payton explained that the network’s strategy was “for-students-by-students”. In many instances, students don’t like to necessarily discuss health related issues that could affect them in everyday conversation. Since social media has become a mainstream of communication for many young adults, I believe this has been a successful way to inform students about the project. I’m looking forward to seeing the positive impact that myHealthImpact is going to make in the lives of college students.
Follow @myhealthimpact on Twitter and tumblr.myhealthimpactnetwork.org on Tumblr.
Share
In Partnership with: Poole College of Management, College of Humanities and Social Sciences, National Science Foundation, Penn State
Take Action, Get Tested: Find Your Local Testing Center Why Get Tested?