myHIN Blog
Category: Health Equity Articles

January 23, 2014
10 Ways to Impact Your Health from @myHealthImpact
1) Find a medical doctor who cares and you feel comfortable with sharing your medical history.
2) See your doctor once a year.
3) Get the appropriate medical tests and screenings done (e.g., HIV, blood pressure, bone density).
4) Document your medical history.
5) Know your family medical history; talk to family members about your and their health.
6) Consider using technology to track your health goals (calorie intake, exercise times, types of exercises, weight loss, calories burned, etc.).
7) Get a good night’s sleep.
8) Estimate portion sizes for what you eat.
9) Check condoms for expiration date which is provided on the packaging.
10) Keep a positive spirit.

Share

January 16, 2014
5 Ways to Create a Healthy Lifestyle
With the New Year, I wanted to create a healthy lifestyle I could maintain throughout the year. It is important to set yourself up for success with a clear mind and body. With that said, I developed 5 easy ways to create a healthy lifestyle.
1. Exercise Daily
If you want to live well and live longer, you must exercise! Try to exercise at least 30 minutes a day. Whether it’s going to a gym class on campus or going on a jog at your local park, there are plenty of ways to incorporate exercise in our daily routines. Try walking to class instead of taking the bus, or joining an intramural sport team. Studies show that just 10 minutes of exercise makes a difference—so do something!
2. Be a picky eater!
Set yourself up for success! Think about planning a healthy diet as a number of small, manageable steps rather than one big drastic change.
Focus on finding foods you love and easy recipes that incorporate a few fresh ingredients.
Eat in moderation. Moderation means eating less than we do now. It doesn’t mean you eliminate the things that you love. Just try to eat more healthy things than unhealthy ones. Also think smaller portions. For example, when dining out, choose a starter instead of an entree, split a dish with a friend, and don’t supersize anything. When at home, use smaller plates, think about serving sizes and start small.
Eat breakfast! Eating fruits and whole grains in the morning can help jumpstart your metabolism and energy for the day.
Avoid eating at night! Try to set a time where don’t eat after. Eating late at during a time when you are less active, can cause weight gain and create unhealthy habits. Studies show that after-dinner snacks tend to be high in fat and calories. So avoid them!
3. Get a good night’s sleep
Keep a regular sleep schedule. Set a regular bedtime and wake up at the same time every day. Nap to make up for lost sleep, but make sure to be smart about napping. While napping can help you recharge, it can also create bad habits when it comes to your sleep cycles. Lastly, create a relaxing sleep environment. Make your room more sleep friendly. Keep the noise down, keep your room cool, and make sure that your bed is comfortable!
4. Keep Healthy Relationships
The healthiest people are those who have relationships with other healthy people. Healthy relationships reduce stress, unhealthy habits, and help motivate you to succeed and do better. Surround yourself with people who are going to uplift you and make you feel better about yourself. Having a strong foundation is essential to life.
5. Give yourself a break!
Find fun activities for you to do to relieve stress! Go to the movies or go shopping. Create new hobbies. Hang out with your friends. Do anything that makes you feel happy. It’s important for you to take a break from life’s stresses and create awesome memories.
Follow us at tumblr.myhealthimpactnetwork.org (Tumblr)
Follow us on twitter @myhealthimpact
Share

October 21, 2013
Health Literacy?
Health Literacy is defined as the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions. It requires a complex group of reading, listening, analytical, and decision-making skills, and the ability to apply these skills to health situations. For example, it includes the ability to understand instructions on prescription drug bottles, appointment slips, medical education brochures, doctor's directions and consent forms, and the ability to negotiate complex health care systems. When patients are faced with complex information and treatment decisions, there are specific tasks that should be carried out to ensure that one is getting the best treatment possible. Those tasks include:
• Evaluating information for credibility and quality
• Analyzing relative risks and benefits
• Calculating dosages
• Interpreting test results
• Locating health information.
In order to accomplish these tasks, individuals may need to be:
• Visually literate
• Computer literate
• Information literate
• Numerically or computationally literate
• Oral language skills are important as well.
In addition to that, it is important for patients to articulate their health concerns and describe their symptoms accurately. They need to ask pertinent questions, and they need to understand spoken medical advice or treatment directions. In an age of shared responsibility between physician and patient for health care, patients need strong decision-making skills.
Next time you visit your local physician, make sure you are practicing and carrying out these tasks. It is important for patients to receive the best care possible, as well as, know how to make accurate decisions when it comes to healthcare.
Follow us on Tumblr tumblr.myhealthimpactnetwork.org
Follow us on Twitter @myhealthimpact
Share

August 28, 2013
Unconscious Bias and Your Health
Almost one year ago, I presented to a group of black female college students on the topic, “You Ain’t Crazy: It’s Your Mental Health”. The sisters wanted to have a frank discussion around dealing with the stress associated with day-to-day issues, such as matriculation at a predominately white institute, culture, family, sexism, racism and how life plays out. Responding to the pressures of it all, one student was asked why did she seek help with her issues, and her response was simple: “to make sure that I don’t go crazy”. One point of frustration highlighted by these students was the interplay between perception and reality. There was the constant practice of second guessing their decisions, particularly scenarios dealing with race and culture. After all, who wants to read more into a situation than is there? You know the questions: “Did he mean to say that? What does he mean? How should I take what was said? How would you perceive that?”
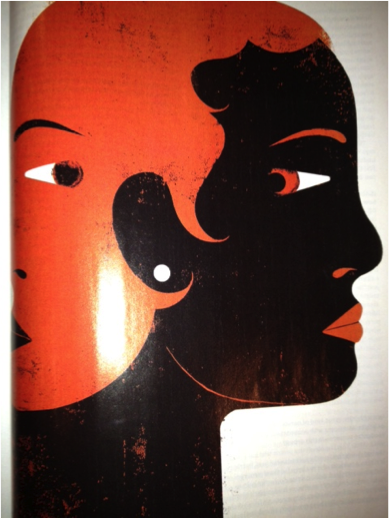 Reading the situation is a complicated topic, or is it? Dr. David R. Williams, professor of sociology and public health, discusses the topic of unconscious bias in the lives of Black Americans in the September 2013 issue of @essencemag. The two-face depiction captures the article’s title, “No, You’re Not Imagining It”. Williams offers a myriad of scenarios that often causes pause. That is, as a Black person, “Is this really happening to me?”. The element of surprise can grip Black folks though the bias imparted by whites can be unintentional. Yet, the outcome or reality of the scenario can have a profound effect on the recipient. Scholars define unconscious bias as the understanding that people can consciously believe in equality while simultaneously acting on subconscious prejudices they are not aware of.
Reading the situation is a complicated topic, or is it? Dr. David R. Williams, professor of sociology and public health, discusses the topic of unconscious bias in the lives of Black Americans in the September 2013 issue of @essencemag. The two-face depiction captures the article’s title, “No, You’re Not Imagining It”. Williams offers a myriad of scenarios that often causes pause. That is, as a Black person, “Is this really happening to me?”. The element of surprise can grip Black folks though the bias imparted by whites can be unintentional. Yet, the outcome or reality of the scenario can have a profound effect on the recipient. Scholars define unconscious bias as the understanding that people can consciously believe in equality while simultaneously acting on subconscious prejudices they are not aware of.
Williams and other public health scholars have determined that the outcome is not a mere sense of challenge of the parts of Black people. As noted in the Essence piece, someone who  fosters and imparts racial prejudices can do so implicitly; though often automatic, the unconscious bias behavior leads to differential treatment – without effort. Unconscious bias influences the lives of Black people in the form of employment (hence, economic), educational and yes, health and health disparities – albeit heart disease, hypertension, diabetes, obesity, engagement in sexual risk behaviors and depression. While the scenarios offered by Dr. David R. Williams represent every day life as we move about, the resulting questions are commonplace but thought-provoking: “Do you see me? “, and if you do, “how do your see me? In health care, public health scholars ponder the same questions. The relevance here is how you see me starts the dialogue of how your treat me as a person and as a patient.
fosters and imparts racial prejudices can do so implicitly; though often automatic, the unconscious bias behavior leads to differential treatment – without effort. Unconscious bias influences the lives of Black people in the form of employment (hence, economic), educational and yes, health and health disparities – albeit heart disease, hypertension, diabetes, obesity, engagement in sexual risk behaviors and depression. While the scenarios offered by Dr. David R. Williams represent every day life as we move about, the resulting questions are commonplace but thought-provoking: “Do you see me? “, and if you do, “how do your see me? In health care, public health scholars ponder the same questions. The relevance here is how you see me starts the dialogue of how your treat me as a person and as a patient.
As I reflect on recent life circumstances, I ponder my own moments of unconscious bias experiences. There I am in the supermarket as I shop for the next family dinner. The checkout clerk pauses, looks and proceeds to ask me: “Why is your hair so short? Are you a cancer patient, or are you making a statement?” Now, the picture shown here is not I, but the style is one that I own. I am not making a statement nor am I a cancer patient. The politics, bias and perceptions of Black hair, particularly for Black women, is a subject reserved for a read of Dr. Lynette Kvasny’s blog, Black Women’s Love Affair with Hair”. Yet, the very question and judgment (“or making a statement, cancer patient) speaks volumes. My response to the clerk was “what if I am a cancer patient?” His apologetic comments followed as I completed my transaction.
shop for the next family dinner. The checkout clerk pauses, looks and proceeds to ask me: “Why is your hair so short? Are you a cancer patient, or are you making a statement?” Now, the picture shown here is not I, but the style is one that I own. I am not making a statement nor am I a cancer patient. The politics, bias and perceptions of Black hair, particularly for Black women, is a subject reserved for a read of Dr. Lynette Kvasny’s blog, Black Women’s Love Affair with Hair”. Yet, the very question and judgment (“or making a statement, cancer patient) speaks volumes. My response to the clerk was “what if I am a cancer patient?” His apologetic comments followed as I completed my transaction.
Case 2: I had a medical procedure done which was a high stress experience . The waiting for the test results was heave, scary and a prayerful time. During the film read with a physician, I stated aloud” “the mass has a meniscus”. To which the physician replied, “how do you know that? How do you know meniscus? How do you know this? This surprises me”. His surprise momentarily precluded the focus on my medical care. My simple reply to his disbelief was “Chemistry 101 Lab and can we focus on my health”.
Then, there is the unconscious bias imparted in the workplace, the unconscious  organizational impact. This level of bias creates an organizational culture that permeates bias rather intentional or unintentional. This mini-me culture can reinforce bias. This can create personal stress particular in hostile workplace environments. The “I understand; I am sorry”, conjectures do little to offer individual support or reduce health stressors. As one sister indicated in that August 2013 session, “Don’t let them steal your joy”.
organizational impact. This level of bias creates an organizational culture that permeates bias rather intentional or unintentional. This mini-me culture can reinforce bias. This can create personal stress particular in hostile workplace environments. The “I understand; I am sorry”, conjectures do little to offer individual support or reduce health stressors. As one sister indicated in that August 2013 session, “Don’t let them steal your joy”.
As Dr. David Williams offers in the @essencemag article, there are others ways to confront these scenarios. Taking care of your health tops his recommendations. Be resilient, and visualize positive outcomes. Breathe. Pause. For as much I share this advice, am I talking to myself? Yes, constantly. After all, it is my (@myhealthimpact) physical and mental health to protect.
Share

July 14, 2013
Representations of Black Womanhood: Implications in Health
Miami University
Doctoral Candidate
The prevalence of chronic disease for African Americans is substantially higher than their white counterparts. According the National Health Statistics African Americans had higher rates of hypertension, diabetes, and obesity (U.S. Department of Health and Human Services [HHS], 2010). In addition to having a greater risk for chronic disease African Americans experience more complications and endure greater rates of mortality. Although current data indicates that there have been improvements in mortality rates, life expectancy, and disease prevalence, disparities between the races are still substantial.
In the United States data on health disparities is rarely presented in an intersectional manner, edifying race, class, and gender (Kawachi, Daniels, and Robinson, 2005). It is through the use of controlling black female images that the interpellation occurs and health disparities are perpetuated. When individuals connect with images and do not engage them critically we allow dominant hegemonic representations to colonize our minds, shaping our assumptions about ourselves and others (Gauntlett, 2002). The connection between how black women were viewed and the implications it might have on health policy, health education, and individual interaction with the healthcare system has never been directly addressed in health disparity literature. Researchers tend to focus on issues of access emphasizing availability of adequate health insurance, culturally competent healthcare providers, and medical centers (Smedley, 2003). While, addressing issues of access is an important component in reducing health disparities controlling for these factors health disparities still remain.
Controlling for variables such as income, health insurance, and access provides minimal impact on the health of African Americans when matched to white counterparts, so the question must be asked, “why do black women have so many health problems relating to obesity, diabetes, and heart disease?” What part does racist and classist ideological beliefs have on health outcomes? Focusing on the short-comings of health education in regards to enacting positive change in minority communities brings one to the study of black female images. It is through these images that black female identity is viewed and formed, shaping intra-personal and interpersonal development and interaction. The intrapersonal deals with the psychology of the individual delving into how identity and self concept is conceived, and this is important for understanding of how the individual may view self, which provides insight into potential motivations for self-care.
The construction and perpetual use of misrepresentations of black womanhood has left an indelible mark on the American healthcare system. As an African American female the relegation to subservient and deviant roles is assured; for the female staring as the jezebel or the mammy is the best that can be expected. Reiterations of these representations play out on the news, television shows, magazine covers, and movies. Visual, auditory, and social text displaying these controlling images almost seem inescapable. Text provides a specific discourse about race, class, gender, and sexuality, and while the viewer is able to pick and choose the text that he are she interacts with the process of mediating the messages that are received is not entirely possible. Living in a perpetuate world of performance due to the white gaze African Americans loss ‘self’ taking on the embodiment of the oppressor’s image of other. This internalization of mammy or jezebel requires the African American woman to perform her ascribed role. The role of the mammy as it relates to self-care does not allow space for the black woman to acknowledge her mental or physical health. The role of the mammy is to care for the needs of others and sacrifice herself for the good of others. The jezebel on the other hand has no real regard for her health or that of anyone else. Her function is to seek pleasure and satisfy her temporal desires. Both images construct identities disconnected from self in the sense that one is unable to be attuned with what is needed to become and remain well. Likewise, many of the other representations of black womanhood suffer from this lack of attunement due to being conflations of old representations of slavery, reclaimed oppressive images, or images constructed in binary opposition to hegemonic representations of white superiority.
Resolving health disparities becomes far more than simply providing education and access, it hinges on identifying racism and acknowledging the cultural and political power that racist images and narratives have in our social ecological spheres (Shavers, 2006; Sanders-Phillips et. al.). Understanding the intentions and motivations behind health behaviors of the marginalized comes with deep exploration of those oppressing acts and representations that serve to colonize and recolonize (Speight, 2007). A stripping away of oppressor hegemonic cultural narratives must be undertaken and empowered counternarratives constructed from more authentic afrocentric spaces must occur.
Follow us on Tumblr tumblr.myhealthimpactnetwork.org
Follow us on Twitter @myhealthimpact
Share

April 10, 2013
The Problem with Black Women’s Health
Dominant. Independent. Bitter. Empowered. Manipulative. “I can do bad all by myself”. Superwomen. Stubborn. In denial. Ladies, what do these characteristics describe? These words or phrases are often used to label African American women. Whether we categorize these features under positive or negative connotations, there is unfortunately some truth behind every single one of them. African American women are hard- working, dedicated, educated professionals but we tend to put everyone and everything before ourselves. We want the best for our families and friends, which tends to become our overall mission of life, and forget about our own personal image and health. In many cases, African American women are single parents or just self- reliant individuals who metaphorically develop stern, powerful mindsets as their defense from real and perceived attacks. We go hard on ourselves since we automatically fall within the lower rank in American society; being classified as “double wammies” since we are female AND of the racial minority.
The number one health-related issue that black women deal with is cardiovascular disease. According to the National Stroke Association, one half of all African American women will die from stroke or heart disease. The death rates from heart disease and strokes for African American females are double those of White and Hispanic females. Our culture also tends to continuously struggle with health problems associated with obesity and high blood pressure. From overworking ourselves and fighting sleep, to insisting that we are in good health (bitterness), all of these cultural aspects play a role in our refusal of medical assistance when we need it most.
“Too many of us are just as crazy, walking (or running) around in denial, ignoring signs (headaches, exhaustion, dizziness, vision changes, weakness, numbness) that should send us to the doctor, not to the office or the car pool or off on that next ‘all important’ business trip. We are in denial about the real impact of our obesity, our smoking, drinking, and lack of exercise…all women should remember that whatever power we each possess is rooted first and foremost in our health. We work so hard to control so much and we’re always up for a challenge. Fine! Here’s a challenge! Commit to spending more time and attention controlling—and caring for—yourself.” (Caroline Clarke, Black Enterprise: Wealth for Life)
Share

September 10, 2012
“You Ain’t Crazy: It’s Your Mental Health!”
On Thursday, August 30th, Dr. Payton gave a presentation on campus titled ‘You Ain’t Crazy: It’s Your Mental Health’ where she discussed mental health issues in the African-American community. What stuck out to me the most was the video she showed featuring Terrie Williams where she talks about her book “Black Pain: It Just Looks Like We’re Not Hurting”. Williams talks about how people think they are the only one who is going through something so they keep things bottled in and suffer from depression, hyper tension, and heart disease; or it will come out through self-medicating, gambling, sex, risk behaviors, etc. Risk behaviors can only increase the chance of being exposed to HIV.
For some strange reason, in our community, when we are suffering from something such as depression, we don’t go and get help. Instead, we turn to a friend who ends up giving us bad advice or just decide to seek a spiritual source to resolve our problems. While I am not knocking the latter, sometimes it is good to keep mental and spiritual health issues separate. Unfortunately, I am speaking from experience.
Last semester I had things going on with my family that I had never experienced before and I didn’t have time to react properly. I used my school and extra-curricular activities as a way to block everything out until one day it caught up with me. I literally woke up crying. I didn’t go to class that morning (which added to my stress) and I reached out to one of my sorority sisters who I am close with. Having experienced depression before, she forced me to go to the University Health Center to seek counseling. I was skeptical at first, but I figured it wouldn’t hurt to talk to someone who was a professional. I went to the Health Center and was told that I needed to set up an appointment. I was upset because I didn’t want to wait to talk to someone in seven days; I needed someone at that moment. I was afraid that my natural habit of pushing things away would hinder me from receiving proper help. In any case, I set the appointment and returned a week later. Unfortunately, the counselor was not helpful, but I was proud of myself for taking the initial step.
When I told certain people in my family that I went to see a counselor their response was ‘what do you need to do that for?’. I responded ‘to make sure I don’t go crazy!’. I also told them that I wanted to find another counselor and begin seeing them regularly, again they asked ‘what do you need to do that for?’. I believe that counseling can help you receive an unbiased opinion on how you should move forward. A counselor does not give you advice based on experience. They give you advice based on clinical research that can help you control your reaction to events that you can’t control. Can you control risk behaviors?
If you’re reading this and you have something that you are dealing with, seek help. More than likely you are not alone in the matter. If you need motivation, watch the video below featuring Terry Williams who also gives her personal testimony about battling with depression.
For up-to-date information, follow @myhealthimpact on Twitter!
Share
In Partnership with: Poole College of Management, College of Humanities and Social Sciences, National Science Foundation, Penn State
Take Action, Get Tested: Find Your Local Testing Center Why Get Tested?